Translate this page into:
Importance of orthodontic movement in interdisciplinary treatment for restoring esthetics and functional occlusion
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
This article describes interdisciplinary treatment conducted in adult patients, 49-year-old, with periodontal problems, losses and dental inclination, occlusal trauma, localized bone loss, and necessity of rehabilitation with dental implants. Alignment and leveling of the teeth, the molars uprighting with cantilever, and space closure were performed the treatment was facilitated by periodic periodontal control. The resultant occlusion was stable throughout a 5-year retention period. In conclusion, interdisciplinary treatment combined with periodontics, orthodontics, implantodontist, and restorative dentistry was useful for improving the patient’s oral health, function, and esthetics.
Keywords
Adult
orthodontic appliance
tooth movement
INTRODUCTION
Interdisciplinary treatment plans for patients with large edentulous spaces in the molar áreas. Adults needing comprehensive orthodontic therapy often have dental and periodontal problems. Saga et al.[1] described several common sequelae of missing mandibular first molars such as tipping and drifting of adjacent teeth, poor interproximal contacts, poor gingival contour, reduced interradicular bone, and super eruption of unopposed teeth.
Demand for orthodontic treatment of adult patients has become common in the past 20 years. Treatment in this population is the fastest growing subspecialty area in orthodontics. The major reasons for this increase are improvements in orthodontic appliances and in adults greater awareness of the availability of treatment, understanding of how orthodontic treatment can augment other dental treatments, and social acceptance of orthodontic appliances.[2]
Orthodontic treatment in adults requires awareness that they have unique intraoral characteristics, such as compromised periodontal health. This situation may be due to physiological wear of teeth; poor oral hygiene; or loss of teeth, leading to premature; and inadequate contacts. Orthodontists need to be attentive to these problems in order that patients’ expectations do not exceed the care that can be offered.[3]
Among the most common dental problems present in adults are molar tipping due to tooth loss. The tipping can lead to occlusal trauma, food impaction, changes of bone anatomy around the tipped tooth, and compromise of edentulous spaces for future prosthetic rehabilitation.[4]
One of the fundamental techniques used in orthodontics is that of molar uprighting with the use of uprighting springs.[5] In this case report, we describe the use of uprighting springs as part of an interdisciplinary treatment.
DIAGNOSIS AND ETIOLOGY
A 49-year-old woman was referred for restore prosthetic spaces that were committed mainly by mesial movement and tipping of the second molars and for correction of mandibular anterior crowding and thus reinstates their esthetics and function. Her medical history did not contribute to underlying systemic conditions. The temporomandibular joint examination was normal, with an adequate range of jaw movements. The pretreatment facial examination showed a hyperdivergent facial pattern with a convex soft-tissue profile, the frontal view was almost symmetrical and passive lip seal [Figure 1].

- Pretreatment facial and intraoral photographs
The intraoral examination showed the canines were in a Class I relationship bilaterally, but the molar relationship could not be established. Spaced arches were observed in the both dentitions because of the missing four first molars overjet and overbite were adequate. Presence mandibular anterior crowding, mesial movement, and tipping of the second molars. The maxillary and mandibular dental midlines were coincident with the facial midline [Figure 2].

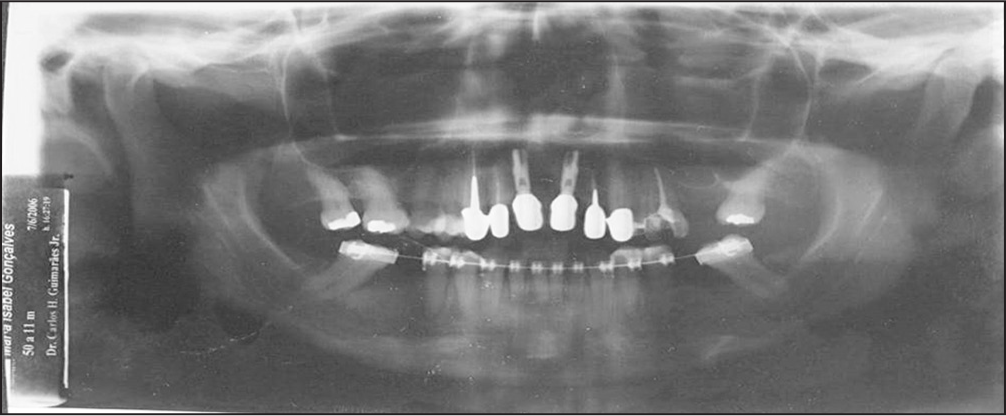
- Pretreatment panoramic radiograph
The panoramic radiograph revealed the missing teeth, implants in maxillary central incisors, endodontic treatment of teeth 12, 13, 22, and 25, restorations, extrusion and mesial tipping of the mandibular second molars, with bone loss in the mesial of these teeth [Figure 3]. Cephalometric analysis indicated a skeletal Class I, protrusion of the maxillary incisors, and good positioning of the apical bases [Figure 4].

- Pretreatment cephalometric radiograph

- Cantilever of titanium molybdenum alloy to second mandibular molars upright
Treatment objectives
The treatment objectives established for this patient were:
Periodontal control,
Alignment and leveling of the mandibular anterior teeth,
Verticalization of the mandibular second molars with cantilevers, and
Re-establishment of the prosthetic spaces correcting abutments for fixed prostheses and implants.
Treatment alternatives
Based on the treatment objectives, the following treatment alternatives were presented to the patient:
Verticalization of the second molars with cantilevers and space opening for the teeth 26, 36, 36, and subsequent rehabilitation with implants;
Verticalization of the second molars with mini-implants and space opening for the teeth 26, 36, 36, and subsequent rehabilitation with implants; and
Verticalization of the second molars and total closure of the spaces with mini-implants.
The patient rejected the second option for this option to be more invasive and rejected the third option because of the long treatment period required.
Treatment progress
After the diagnosis established, a multi-disciplinary treatment plan was developed. The plan included contributions from orthodontics, periodontics, implant dentistry, and prosthetics, the treatment plan began with definition of which teeth would be essential for the prosthetic treatment. Then, a mandibular fixed appliance was bonded (slot0.022-in MBT-Abzil, 3M Unitek, Monrovia, Calif). Initially, alignment was started with a 0.014-in thermalactivated.
After 4 months, a maxillary fixed appliance was bonded with the intent of closing the space of the right first maxillary molar and opening the space for rehabilitation of the left first maxillary molar. After that a posterior occlusal adjustment was performed to remove undesirable contacts caused by mesial tipping of the right second mandibular molar. The second mandibular molars were uprighted with a 0.017 × 0.025-in cantilever of titanium molybdenum alloy [Figure 5]. After the alignment and leveling of the mandibular arch, the lower fixed appliance was removed, and removable retainer was installed; this type of retention was chosen because the patient was being referred for prosthetic rehabilitation. After rehabilitation, the 3 × 3 retainer was bonded.

- Posttreatment facial and intraoral photographs
The second treatment phase consisted of periodontal monitoring. Through probing and radiography, the maxillary and mandibular dentoalveolar remodeling at the mesial aspect of the uprighted molars could be seen. After completion of the orthodontic treatment and correction of malocclusion, dental implants, and fixed prostheses were installed. The orthodontic treatment required about 18 months.
Treatment results
The posttreatment facial photographs show that a proper facial profile was maintained the initial Class I dental relationship was maintained. The collapse in the posterior occlusion caused by tipping and mesial movement of the mandibular second molars was corrected [Figure 5].
In the panoramic radiograph, the 3 dental implants and complete mesialization the first right maxillary molar are shown, beyond dentoalveolar remodeling owing to orthodontic movement, and the periodontal control [Figure 6]. Posttreatment cephalometric evaluation showed little changes in the skeletal variables. The Class I jaw-base relationship was kept, the mandibular plane angle was stable and changes in the inclinations of the incisors were not observed [Figure 7].
- Posttreatment panoramic radiographs

- Posttreatment cephalometric radiographs
From the orthodontic treatment associated with periodontal and prosthetic rehabilitation, interferences in occlusal balance were removed and a stable posterior occlusion was achieved centric relation and centric occlusion were established associated with a lateral disocclusion by group function bilaterally. The installed prostheses and implants remained steady through the last follow-up visit, five years after completion of treatment [Figure 8].

- Postretention facial and intraoral photographs
DISCUSSION
There have been various reports of successful morphologic and esthetic changes after interdisciplinary treatment in adults patients, especially in patients with loss of teeth and periodontal breakdown cause pathologic migration of teeth.[1,6-8] Such patients should be treated with an interdisciplinary approach aimed not only to improve oral function and esthetics but also to prevent such problems later in life.[4] In the case reported, the treatment restored to the patient function, esthetics, and improved periodontal condition.
Many studies have demonstrated that orthodontic treatment can improve the periodontal situation in patients with pathological migration, providing improved function and esthetics.[4] Many investigators have concluded that infra-bony defects, when orthodontically moved, can change the morphology of the defects, reduce the probing depth, and resolve the radiological bone defect.[1,9,10]
In patients with periodontal involvement, periodontal therapy preceding the orthodontic treatment usually is recommended, based on the belief that orthodontic treatment in the presence of inflammation may lead to irreversible rupture of the periodontium.[11] Some authors also add that it is advantageous to wait 4-6 months between treatments in order to ensure that orthodontic treatment will be performed with healthy tissues and to determine if the patient’s motivation and hygiene habits are appropriate.[12,13] In this patient, before orthodontic treatment was begun, periodontal therapy was performed, with subgingival scaling and evaluation of the depth of infra-bony pockets, especially in the mesial aspect of the molars that had undergone verticalization.
Impacted molars or mesially or lingually tipped molars require verticalization. This can be achieved through several approaches, including Australian uprighting spring, cantilever spring, NiTi coil spring, mini-implants, forced eruption by elastics, traction with removable appliances, and surgical uprighting.[14-16] Any of these techniques can achieve verticalization of tipped teeth in specific situations. The choice of any of them is determined on the severity of the tipping, the accessibility to the coronal surface, the undesirable side effects, and the simplicity and convenience of the verticalization mechanics.[5,17]
In this patient, we chose uprighting of the mandibular second molars with the aid of verticalization springs, mainly because it was the least invasive option, and also because it imposed no additional charges. In this uprighting technique, a canine and a premolar tooth act as anchorage teeth and are connected with the wire.[18] Added to this, the arm of the verticalization spring is bent to the lingual side to prevent buccal movement of the anchored tooth that are to be uprighted. Thus, the bend of the arch has been used in several orthodontic dental movements.[19,20]
During the movement of the teeth involved in the verticalization mechanics, light forces were used, especially because the teeth had periodontal compromise. In teeth with periodontal disease, alveolar bone loss results in apical displacement of the center of resistance; thus, it is important to use only light and controlled forces in order to minimize insertion loss and root resorption.[16]
Our management of this patient was based in part on literature reports that encourage orthodontic treatment of patients with periodontal disabilities, since such treatment can facilitate control and monitoring of the inflammation. Research has shown that orthodontic dental movement is a stimulating factor for bone apposition. Furthermore, increased bone healing after orthodontic movement in areas of periodontal defects has been reported.[21]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Treatment of an adult with several missing teeth and atrophic old mandibular first molar extraction sites. Am J Orthod Dentofacial Orthop. 2011;140:869-78.
- [Google Scholar]
- Managing complex orthodontic problems: The use of implants for anchorage. Semin Orthod. 1996;2:153-60.
- [Google Scholar]
- Multidisciplinary management including periodontics, orthodontics, implants, and prosthetics for an adult. Am J Orthod Dentofacial Orthop. 2012;142:235-45.
- [Google Scholar]
- Molar uprighting with the piggyback buccal sectional arch wire technique. Am J Orthod Dentofacial Orthop. 1991;99:276-80.
- [Google Scholar]
- Interdisciplinary orthodontic treatment for a patient with generalized aggressive periodontitis: Assessment of IgG antibodies to identify type of periodontitis and correct timing of treatment. Am J Orthod Dentofacial Orthop. 2015;147:766-80.
- [Google Scholar]
- Interdisciplinary treatment of a nonsyndromic oligodontia patient with implant-anchored orthodontics. Am J Orthod Dentofacial Orthop. 2014;145(4):S136-47.
- [Google Scholar]
- Interdisciplinary treatment of a periodontally compromised adult patient with multiple missing posterior teeth. Am J Orthod Dentofacial Orthop. 2014;145:238-48.
- [Google Scholar]
- Use of orthodontic therapy to alter infrabony pockets 2. Int J Periodontics Restorative Dent. 1990;10:198-207.
- [Google Scholar]
- Reduction of gingival recession following orthodontic intrusion in periodontally compromised patients. Orthod Craniofac Res. 2004;7:35-9.
- [Google Scholar]
- Interrelationship between periodontics and adult orthodontics. J Clin Periodontol. 1998;25:271-7.
- [Google Scholar]
- Clinical implications of recent orthodontic-periodontic research findings. Semin Orthod. 1996;2:4-12.
- [Google Scholar]
- Managing treatment for the orthodontic patient with periodontal problems. Semin Orthod. 1997;3:21-38.
- [Google Scholar]
- Periodontal conditions in patients after molar uprighting. J Prosthet Dent. 1980;43:156-62.
- [Google Scholar]
- Disturbed eruption of the lower second molar: Clinical appearance, prevalence, and etiology. ASDC J Dent Child. 1988;55:114-8.
- [Google Scholar]
- Molar uprighting by a nickel-titanium spring based on a setup model. Am J Orthod Dentofacial Orthop. 2014;146:119-23.
- [Google Scholar]
- Bone stress and strain after use of a miniplate for molar protraction and uprighting: A 3-dimensional finite element analysis. Am J Orthod Dentofacial Orthop. 2014;146:198-206.
- [Google Scholar]
- A numerical simulation of tooth movement produced by molar uprighting spring. Am J Orthod Dentofacial Orthop. 2007;132:630-8.
- [Google Scholar]
- Mandibular canine intrusion with the segmented arch technique: A finite element method study. Am J Orthod Dentofacial Orthop. 2015;147:691-7.
- [Google Scholar]
- Bone apposition in surgical bony defects following orthodontic movement: A comparative histomorphometric study between root-and periodontal ligament-damaged and periodontally intact rat molars. J Periodontol. 2004;75:1013-9.
- [Google Scholar]