Translate this page into:
Multidisciplinary treatment in a patient with temporomandibular disorder
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Adult patients with a multitude of problems require seamless integration of interdisciplinary protocols. This article presents a case of an adult female who reported with temporomandibular disorders, a crossbite and a Class III skeletal pattern. An interdisciplinary approach using expansion and surgery was used to treat the condition, followed by an esthetic/restorative protocol, achieving excellent results.
Keywords
Class III
esthetics
hyrax
interdisciplinary
surgery
INTRODUCTION
Most of adult patients who seek orthodontic treatment need some kind of interdisciplinary intervention.[1-3] Also to the esthetic requirements often requiring the integrated participation of orthodontics with other disciplines, functional requirements are also needed at several instances during this integration. There are cases where missing teeth, functional disorders, skeletal abnormalities, and other irregularities are present. In such cases, the seamless integration among specialties is absolutely necessary for successful treatment.[4-6] Failure to observe these interrelated factors can lead to inaccuracies in the acquirement of the diagnosis which in turn leads to failure of therapeutic procedures that may impair treatment and worsen the initial problem. The preparation of a list of problems that takes into account the strong link that function is associated with esthetics is fundamental for the implementation of planning and treatment. At the same time, an assessment should be carried out of existing characteristics and situations that are positive and inherent and should not be changed by the treatment. Thus, the needs assessment, especially in adult patients, should start from the outside in.
In other words, one must evaluate the facial, oral and dental structures, in this order, because the perception and evaluation of the whole face is more developed (instinctive) in most people when compared to parts on their own such as lips, smile, and teeth. In addition, the morphogenetic facial pattern maintains a relationship with the dentoalveolar complex, influencing it and giving clues to its anomalies.[7] With the relationship information that each structure keeps in itself, the diagnosis is formed, and a plan is prepared.[8-10] This assumption is important since, orthodontic treatment has its limitations in the treatment of adults, requiring dental compensation or decompensation. The dental execution of the limits of orthodontics in adults is determined by the existence or non-existence of facial balance and by orthopedic needs since these patients no longer depend on growth. When there is a lack of harmony and balance in facial structures, orthodontics must recognize its limits and seek integration with other disciplines that can help in troubleshooting. A good example can be seen in treating jaw expansion. Although rapid maxillary expansion is a safe procedure and has been tested in children and adolescents since Haas[11] established the use of the fixed palatal expander in the 1960s, its use is not recommended without surgical assistance in adults.[12-14] Surgeries such as the Le Fort subtotal segmental osteotomy[13,15] and lateral and midline maxillary osteotomies,[14-18] together with fixed palatal expanders, have been used successfully to allow for the opening of mid-palatal sutures and maxillary enlargement, becoming an integral part of the planning of maxillary atresia treatment in adult patients. Orthodontics is also limited in oral and dental problems. The possibility of restoring tooth structure is beyond the orthodontic scope. Integration with other specialties that are specific for this purpose, such as prosthetics is necessary whenever a restorative and/or esthetic treatment requires it. Thus, it is our aim to present a clinical case in which integrated treatment philosophy is fundamental to the success of the final result.
CASE REPORT
Etiology and diagnosis
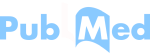
A 28-year-old female patient went to the orthodontist with signs and symptoms of temporomandibular disorder (TMD) and with cosmetic treatment history in the upper anterior region for anterior crossbite correction. She reported that after completion of these earlier restorations she began to have biting difficulty because her teeth only touched the anterior region. She was dissatisfied with the esthetic appearance of her teeth and the discomfort caused by the restorations while biting. During the physical examination, an anterior prematurity was found, which led to the emergence of open bite in the posterior region [Figure 1]. The difficulty to occlude the posterior teeth led to a consequent difficulty in chewing, if did not occur, at the least worsened signs and symptoms of TMD.

- Pre-treatment intraoral photographs showing anterior premature contacts
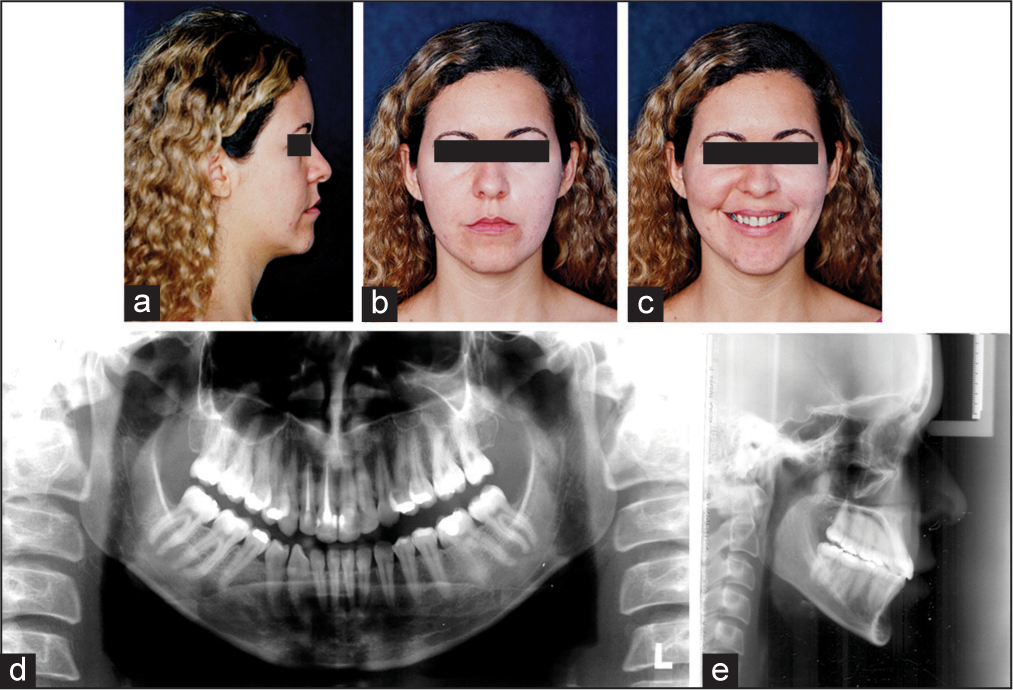
Occlusal, skeletal, functional and esthetic problems were observed on physical examination, where extra-oral photographs, panoramic X-rays, and teleradiology aided in the diagnosis [Figure 2]. In the full assessment of the patient, we may draw up a list of problems, which begin with the Class III skeletal and dental relationship, where the problem was found in the retruded maxilla, leading to a concave profile with zygomatic projection deficiency and near absence of infra-orbital depression. The maxillary atresia also created a bilateral posterior crossbite. Furthermore, the maxilla was transversely inclined, the inclination of the anterior and posterior occlusal plane with the presence of a left posterior open bite. In the cephalometric analysis, an ANB angle of 0 was found [Figure 3]. Also to the skeletal problems, there were also the dental problems with functional and esthetic involvement.
- Pre-treatment extraoral photographs and radiographs
- Pretreatment lateral tracing
The inferior dental midline had a 2 mm deviation to the right. There was the presence of previous diastema in the lower arch, unevenness of the cervical edge, uneven incisal edges of the upper lateral incisors and composite resin restorations that were deficient in the four upper incisors. The restorations of the upper incisors, as previously mentioned, in addition to causing a previous anterior prematurity, had esthetic deficiencies that needed to be corrected. While smiling the influence of skeletal and dental effects in its esthetics became evident. A wide buccal corridor was a consequence of maxillary atresia and uneven incisal edges caused by maxillary inclination [Figure 4].

- Pretreatment photograph showing wide buccal corridors
Treatment objectives
After compiling the list of problems, the treatment objectives were elaborated following certain priorities. The maxillary problems were the first to be evaluated since several facial and occlusal problems originated from maxillary retrusion and atresia. The need for maxillary expansion and advancement led to the surgical option. It was established that surgically assisted expansion would be the first intervention to be performed since the possibility of side-effects from the expansion, as well as forward and lower movement of the jaw, could be beneficial to the treatment.[19] Although these effects could be temporary,[20,21] the possibility of maintaining them with the cooperation of the patient using Class III elastics was plausible. Therefore, the activation of the expansion screw and posterior expansion should have been as large as possible to maximize side-effects. Obtaining maxillary advancement would provide an improvement in the relationship between the jaw and mandible, having positive functional and esthetic consequences. Occlusion would benefit from the correction of overbite, overjet, posterior cross bite and the profile would incline towards a better balance and facial harmony. The remaining orthodontic needs, such as midline deviation, alignment, leveling and closing of dental spaces, would be corrected with fixed appliance/braces. Esthetic correction of the previous composite resins would be made at the end of orthodontic treatment.
TREATMENT ALTERNATIVES
Maxillary deficiency influenced facial harmony in the three planes. Their retrusion, atresia, and inclination led the focus of treatment to the correction of these problems. For being an adult patient, all treatment alternatives went through surgical procedures. There were two possibilities. The first would be a combination of a surgically assisted expansion prior to orthognathic surgery of the maxillary advancement, and the second would be a correction of all irregularities in a single surgical procedure. It was agreed with the patient that the first alternative would be chosen, even with the possibility of two surgical procedures, since the chance of improved relations of the jaw after the expansion were real. The side effects of the expansion could be utilized with the collaboration of the patient (using elastics) for the retrusion and inclination solution of the maxillary plane. As regards to the replacement of upper incisor restorations, which type of procedure would be done would be decided after the orthodontic treatment. The possibility of direct or indirect restorations would be decided at an opportune moment.
ORTHODONTIC AND SURGICAL TREATMENT
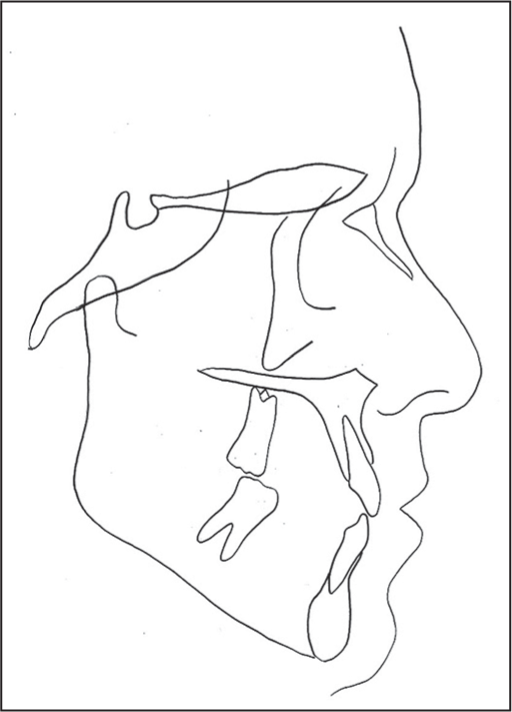
The treatment started with the assembly of the hyrax expansion device and followed up with expansion surgery. Immediately after the surgery the expansion screw was activated four times and closed again so that the effectiveness of the breaking strength of the sutures and osseous columns was verified. The activations were initiated 24 h after surgery, and the expansion screw was turned for four quarter turns per day (1 mm) for 10 days. The activation was implemented up to the expansion screw’s limit. The intention was to get the maximum amount of expansion possible was performed [Figure 5]. During the contention phase, which was carried out maintaining the hyrax appliance in position, there as a complete assembly of the lower fixed appliance and partial assembly of the upper fixed appliance. In the lower arch, the intention was to not allow for the protrusion of the incisors. For this, the entire lower arch was contained via laceback. In the upper arch, we waited for spontaneous partial recurrence of the incisors for the complete assembly of the appliance. The standard edge-wise fixed appliance was used [Figure 6]. With the clinical evaluation of the orthopedic effects of the expansion, it was found that the jaw had expanded and advanced. At this point, it was decided that orthodontic camouflage would be used instead of decompensation for orthognathic surgery of maxillary advancement.

- Post expansion intraoral photographs
- Contention period of expansion and start of brace assembly
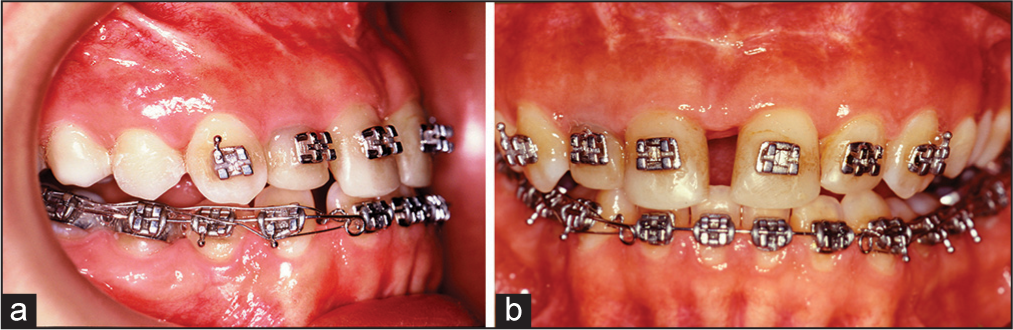
Alignment and leveling of the upper and lower arch were carried out with the following sequence of arches: 0.14″ (niti), 0.16″, 0.18″, 0.20″ and 0.19″ × 0.25″ of steel. During the leveling, Cl III elastics and vertical elastics were used in the right posterior region. The use of vertical elastics was intended to correct the inclination of the occlusal plane. After expansion, there was a large occlusal imbalance where only the second molars were touching. This situation, though undesirable, allowed for an extrusive unilateral mechanism to improve the inclination of the occlusal plane. The patient’s cooperation was excellent, and the desired result was achieved. During the final phase, the remaining spaces were closed with elastic (power) chains and the cervical heights of the upper lateral incisors were evaluated by periodontics since there was a depth discrepancy between the gingival grooves of these teeth [Figure 7].

- Intraoral photographs during and immediate debonding
ESTHETIC RESTORATION TREATMENT
As previously stated, at the end of orthodontic treatment, a gingival height discrepancy was found in the upper lateral incisors. At probing, there was a 2 mm difference between/ among groove depth of the lateral incisors. This groove depth difference ruled out the correction of the gingival level by orthodontic movement, since the problem was periodontal. Surgical correction was performed to create a new gingival zenith contour of the right lateral incisor [Figure 8]. Once the gingival correction was performed and adequate time had passed for scarring and maturation, the fitting/fixing of metal-free porcelain crowns (In-ceram) was planned. This proposal was based on the fact that the right central and lateral incisors already had their canals treated and that the left central and lateral incisors had a concentrated quantity of composite resin. Dental rehabilitation was carried out taking into consideration all compensations caused by the orthodontics. During the assembly of the ceramic crowns, the vestibular contour sought to minimize the visual effect of vestibular inclination of the incisor crowns giving a more curved contour while applying the porcelain [Figure 9].

- Intraoral photographs of the gingival recontouring procedure

- Inceram anterior crowns
DISCUSSION
Treatment of adult patients with esthetic and functional problems involving skeletal and dental deficiencies require integrated multidisciplinary interventions.[1,2] The major challenges in such cases are to define the limits of each specialty and the right moment to put it in practice.[3,4] In this clinical case in which problems in the jaw affected the entire facial harmony, oral and dental, and had to be addressed in an integrated and complementary way to a planning based on the complaint from the patient and the priorities from the list of problems.[5,8,9] The great dilemma that existed was the need for jaw correction in the three spatial planes since the jaw was found to be retruded and tilted. The surgical necessity was evident, but it was not clear what was the best surgical option to take. Explaining better, although the surgical need was a certainty, there was the question of what type of surgery would be ideal. Despite jaw problems being complex, involving three facial planes, the degrees of complexity of each problem were different. The maxillary atresia presumed a prominent position from the standpoint of the deficiency since its relationship to the jaw led to a bilateral crossbite. The retrusion and transverse inclination of the occlusal plane caused more moderate effects, both in profile and tooth exposure. This apparent relativity of the degree of severity of jaw problems influenced the development of a plan that took these factors into consideration. It was decided that surgically assisted expansion would be the preferred option for the correction of the maxillary atresia and an attempt would be made to resolve the retrusion and the transverse tilting of the jaw taking advantage of the side effects of expansion[11-19] and the cooperation of the patient, who would make use of inter-maxillary elastics. If all deficiencies were not resolved, a second surgery would be indicated for advancement and disinclination of the jaw. This option was presented to the patient, and she accepted. Her cooperation was fundamental to the treatment outcomes. The use of elastics proved efficient and combined with the orthopedic effects of the expansion, required for just one surgery [Figure 10].
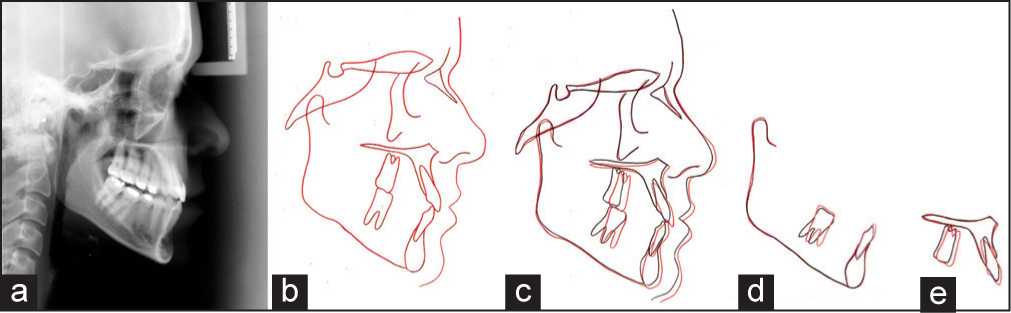
- Post treatment lateral cephalogram and superimposition
The advancement of the jaw, however slight, when coupled with the small tooth movement of the upper incisors (mesial movement and extrusion) was sufficient to correct the overbite and overjet, eliminating premature contact and ending signs and symptoms of temporomandibular disorder (OR TMD), which was one of the patient’s complaints. After completing orthodontic treatment, a periodontal surgery to correct the gingival cervical level of the upper incisors was performed, and metal-free porcelain crowns were made (InCeram). The respective crowns were made following all compensations and dental, oral and facial dimensions. Throughout the correction period of the esthetic restorations, the patient used contentions. The lower contention used was a 3 × 3 bar. In the upper arch, a removable wraparound contention was used.
Multidisciplinary integration was carried out with all due coordination. Respecting the limits and the correct timeframe of execution of each discipline was a decisive factor in obtaining the occlusal, functional and esthetic results of the clinical case, which together contributed to the relief of the signs and symptoms of TMD with the consequent success of treatment and patient satisfaction [Figure 11].
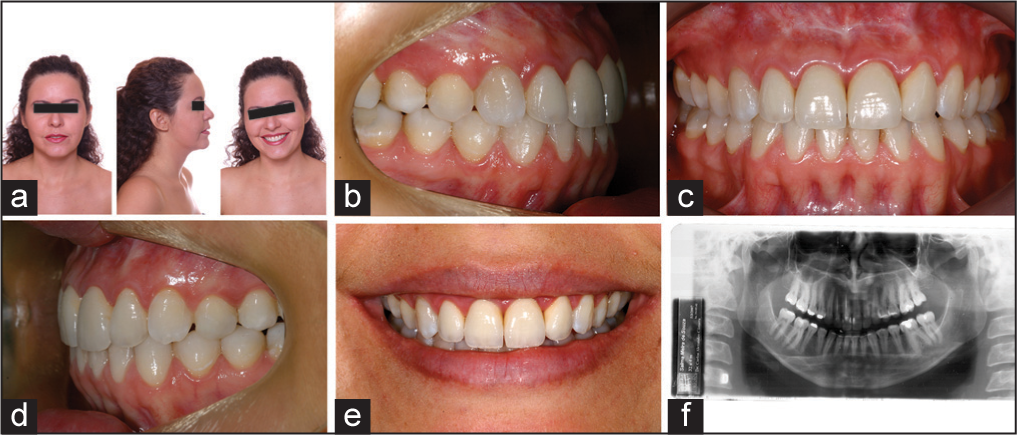
- Post treatment photographs and radiographs
CONCLUSIONS
Integrated dental treatment is critical to cases of adult patients with multiple esthetic and functional problems. The understanding of a multidisciplinary team of the patient’s needs makes the possibility of success much more viable. The report on the clinical case presented demonstrates these precepts, in which the correct observation and intervention of each specialty/discipline was fundamental in obtaining the final result.
References
- Tratamento interdisciplinary — Ajuste estético de casos ortodônticos atípicos. Rev Dent Press Ortod Ortop Facial. 2000;5:68-74.
- [Google Scholar]
- Guidelines for managing the orthodontic-restorative patient. Semin Orthod. 1997;3:3-20.
- [Google Scholar]
- Tratamento integrado de reabilitação oral em paciente adulto. Rev Clin Ortod Dent Press. 2004;3:83-90.
- [Google Scholar]
- Integrated orthodontic, surgical, and prosthodontic treatment of advanced malocclusion. Quintessence Int. 1998;29:659-66.
- [Google Scholar]
- Managing treatment for the orthodontic patient with periodontal problems. Semin Orthod. 1997;3:21-38.
- [Google Scholar]
- Diagnóstico em ortodontia. Maringá: Dental Press; 2004.
- Estética em ortodontia: Parte I. Diagramas de Referências Estéticas Dentais (DRED) Rev Dent Press Estét. 2004;1:40-57.
- [Google Scholar]
- Estética em ortodontia: Parte II. Diagramas de Referências Estéticas Faciais (DREF) Rev Dent Press Estét. 2005;2:82-104.
- [Google Scholar]
- Estética em ortodontia: Diagramas de Referências Estéticas Dentárias (DRED) e Faciais (DREF) Rev Dent Press Ortod Ortop Facial. 2006;11:130-56.
- [Google Scholar]
- Rapid expansion of the maxillary dental arch an nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;1:200-17.
- [Google Scholar]
- Maxillary expansion: Clinical implications. Am J Orthod Dentofacial Orthop. 1987;91:3-14.
- [Google Scholar]
- Surgically assisted rapid palatal expansion: An outpatient technique with long-term stability. J Oral Maxillofac Surg. 1992;50:110-3.
- [Google Scholar]
- Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995;10:75-96.
- [Google Scholar]
- Surgically assisted rapid maxillary expansion in adults. Int J Adult Orthodon Orthognath Surg. 1992;7:37-41.
- [Google Scholar]
- Unilateral and bilateral corticotomies for correction of maxillary transverse discrepancies. Eur J Orthod. 1992;14:110-6.
- [Google Scholar]
- The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;35:200-17.
- [Google Scholar]
- A longitudinal study of skeletal side effects induced by rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 1997;112:330-7.
- [Google Scholar]