Translate this page into:
Laser therapy for faster orthodontic tooth movement
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
One of the major component of patient to reject orthodontic treatment is the long duration of treatment. If Low intensity laser therapy can promote wound healing by increased cell proliferation and improved micro circulation can bring about faster bone remodelling at fracture sites; then why not to use it with orthodontic forces for better results? Soft tissue laser has now become a part of essential equipment of modern dental clinics. To accelerate the physiologic tooth movement during orthodontic treatment a thorough knowledge of laser unit, mode of action and key factors to gain therapeutic effect is a must which this article illustrates. Study carried out by us did show a 30% reduction in the treatment time.
Keywords
LILT
OTM
biostimulation
INTRODUCTION
One of the major concerns to the orthodontic patients is treatment time and second is pain or discomfort. Reducing the treatment time requires increasing the rate of physiologic tooth movement. Many methods have been used in the past to accelerate the orthodontic tooth movement as electric and magnetic stimulation,[1] drug injections of parathyroid hormone, misoprostol (prostaglandin E1 analog), prostaglandin E2 (PGE2).[2,3]
Although these substances stimulate the rate of tooth movement, they also have an undesirable side effects of local pain and discomfort during the injections. Recently, electric stimulation and resonance vibration[4] have been tried in animals, but these methods require an apparatus that is not routinely used in dental practice. To reduce pain during treatment often analgesics are advised. But studies have shown that analgesics inhibit prostaglandins, which in turn slows down the tooth movement.[5]
Low intensity laser therapy
For more than a millennium, dozens of cultures identified light as possessing healing properties. Low intensity laser therapy (LILT), the energy output is low enough so as not to cause a rise in temperature of the treated tissue above 36.5°C or normal body temperature. In initial days, LILT found its application only in medical sciences such as orthopedics, surgery, and medicine.[6]
In the early 1980’s, dental lasers were introduced and recognized as a tool for better patient’s compliance.
Lasers in dentistry
Medical and dental lasers are found in wavelengths in a relatively narrow range within the electromagnetic spectrum. They include the range of visible radiation (400-750 nm) and invisible thermal radiation, which can be further broken down into the near infrared (750-2000 nm), mild infrared (2000-3000 nm), and far infrared (3000-10,600 nm) wavelengths. The illustration in Figure 1 depicts the short span of the electromagnetic spectrum wherein the wavelengths of popular lasers fall.[7]

- Electromagnetic spectrum
Dental lasers can be separated into two broad categories:
-
High-power lasers
High-power lasers typically use above 1.0 watt (W) of power output concentrated in a small, defined area to cut hard and soft tissues.
-
Low-power lasers
Low-power lasers typically use significantly less power than high power lasers, usually ranging from 5 mW up to 400 mW. They are used for caries detection, teeth whitening, light curing of composite resins, oral pain relief for aphthous ulcers, temporomandibular joint disorder, and to increase osseointegration of dental implants.
In the field of orthodontics, LILT has been used to decrease orthodontic pain, and increase bone deposition across the expanded mid-palatal suture.[8] In the last decade, many histological studies have attempted to determine the effect of LILT on the histochemical pathways directly associated with orthodontic tooth movement (OTM).
Low intensity laser therapy’s effect on main cellular component involved in OTM.[9,10]
Low intensity laser therapy can influence osteoclast regulation by effecting enzymatic levels of transforming growth factor-β1, cyclooxygenase-2, PGE2, fibronectin, collagen turnover, and tissue vascularity preservation. These enzymes induce the expression or inhibition of members of the osteoprotegerin/receptor activator of nuclear factor kappa B ligand/receptor activator of nuclear factor kappa B system and subsequently manipulate the differentiation, maturation, and maintenance of osteoclasts.
Key factors for therapeutic effects of laser
Laser attenuation and penetration depth
Van Gemert and Welch[11] reported that the maximum penetration of infrared lasers in “bloodless, unpigmented tissue” is close to 1 cm.
In 1993, Kolari and Aicksinen[12] found laser transmittance of 632.8 and 820 nm wavelengths through skin to be between 2 and 3 mm.
Photobiology
The first law of photochemistry, also known as the Grotthuss-Draper law, states that light must be absorbed by a chemical system in order for photochemistry to occur. In 2001, Sommer et al.[13] stated that perhaps energy density and light intensity were the most important of the biostimulatory factors. To support their claim, the group points to a number of investigators who found that the stimulatory effect of LILT follows the basic Arndt-Schultz law, which states that “small doses stimulate living systems, medium doses impede, and large doses destroy.” Sommer’s et al. also observed that a threshold of light intensity exists and must be reached in order to produce a biostimulatory effect.
Biostimulatory
Effect of phototherapy increased scientific interest in LILT initially through the early work of Mester et al.’s.[6] They concluded that a low powered laser beam would allow for a “biostimulatory” effect that would quicken the therapeutic process.
Timing
Subjects are more readily influenced by LILT in the initial stages of biological response.
Frequency
Multiple applications of LILT produce a greater response than a single dose.[14]
Energy density/dosage
The rule of reciprocity, also known as the Bunsen-Roscoe rule, states that a photochemical reaction is determined by the dose irrespective of the time needed to deliver that dose. Biologic stimulation by LILT follows dose dependency. This was exhibited through bell-shaped curves where every laser wavelength produced a maximum stimulation at a specific dose. Doses greater and less than the optimal resulted in less stimulation. Bell-shaped curves are indicative of dose dependency.
Very few studies in the literature examined the effect of LILT on rate of OTM, and those too are short-term animal studies. In 2004, Cruz et al.[15] were the first to carry out a study on human over a period of 60 days. In our study,[16] in 2011 we evaluated the efficacy of LILT in reducing orthodontic treatment duration and pain. Individual canine retraction by a nickel-titanium closed-coil spring was done in 21 patients with extracted premolars. Experimental side received infrared radiation from a semiconductor (gallium aluminum arsenide [GaAlAs]) diode laser with a wavelength of 810 nm. The laser regimen was applied on days 0, 3, 7, and 14 in the 1st month, and thereafter on every 15th day until complete canine retraction was achieved on the experimental side. Tooth movement was measured on progress models. Each patient’s pain response was ranked according to a visual analog scale. An average increase of 30% in the rate of tooth movement was observed with the low-intensity laser therapy. Pain scores on the experimental sides were significantly lower compared with the control sides.
Low intensity laser therapy equipment
LASER unit
The laser type-semiconductor (GaAlAs) diode laser [Figure 2] emitting infrared radiation with 808 ± 10 nm wavelength operating according to the manufacturer’s recommendations as in Table 1.

- LASER Unit
| Type | Features |
|---|---|
| Origin | LAMBDA SpA Via dell’impresa 36,040 Brendola (VI) — Italy |
| Model | LA3D0001.1 |
| Input of power supply | 100-240 VAC |
| Network frequency | 47-63 Hz |
| Maximum current absorbed by the network | 0.5 A (@230 V) |
| Output of power supply | 12 VDC-8.33A max |
| Supply voltage for the system | 12 VDC |
| Max absorption of the system | 0.6 A |
| Power output on the work point | 0.1-7 W |
| Working conditions | Temperature: 10°C to 30°C Humidity: 30% to −75% Atmospheric pressure: 700/1060 hPa |
| Storage conditions | Temperature: 05°C to −50°C Humidity: 30% to −75% Atmospheric pressure: 700/1060 hPa |
| External connections | Footswitch (optional)+interlock |
| Cooling system | Air |
| Laser class | 3 |
| Weight | 1 kg |
Handpiece
The handpiece has a cylindrical quartz tip of 4 mm2 surface area from where laser beam is emitted. Black color coded needle are used for therapeutic purpose which is attached to handpiece.
Protection glasses
Safety precautions are worn by both the operator and patient provided by the manufactures. The principle risks with laser are associated with eye damage [Figure 3].

- Protection glass and Disposable LASER tips
PROCEDURE
Low intensity laser therapy for analgesic: Two irradiations are done. One irradiation on middle one-third of the canine root on the buccal side and the second on the palatal side holding the laser tip in direct contact with the tissue.
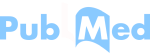
Low intensity laser therapy for biostimulation during OTM: The total of 10 irradiations are done — five on the buccal side and five on the palatal side in order to cover the entire periodontal fibers and alveolar process [Figure 4]. Manual settings of the laser unit shown in Table 2.
- Laser therapy procedure for canine retraction on, BUCCAL. (a) Cervical 1/3rd (b) Middle 1/3rd (c) Apical 1/3rd, PALATAL (d) Cervical 1/3rd (e) Middle 1/3rd (f) Apical 1/3rd
For analgesic purpose, settings adjusted to
|
For biostimulation, the parameters set at
|
World Association of Laser Therapy has laid down standards to carry out study on laser therapy.
LOW INTENSITY LASER THERAPY-MODE OF ACTION
Laser therapy can best be described through its parameters. The core parameters include:
Laser’s wavelength: A laser exists at a specific wavelength, determined by the medium through which energy is pumped to create light.
Modality of application: Laser therapy can be delivered in continuous or interrupted emission modes which is further divided into gated pulsed and free-running pulsed mode.
Power output: Lasers are most easily characterized by the amount of energy they produce, called power output.
Application dose: Application dose measures the amount of energy applied at any one given treatment and is measured in Joules (J).
Treatment dose: The treatment dose, or total energy dose, is an additive value combining the energy delivered over the entire length of treatment.
Energy density: Energy density is a measure indicating the amount of energy received by a given tissue.
Power density: Power density measures the amount of power per unit area leaving the laser applicator or tip.
CONCLUSION
Low-intensity laser therapy increases the rate of OTM in a physiologic manner. It causes no side effects on the vitality or the periodontium of the teeth. Thus, it can safely and routinely be used during orthodontic treatment to shorten the treatment time. Low-intensity laser therapy also is an effective method of analgesia during orthodontic treatment or to relieve from pain immediately after placement of separators.
The Food and Drug Administration does not specify absolute contraindications for the use of LILT. However, individuals have postulated various scenarios in which the therapy should not be used until further research is conducted. One of these is in areas of malignancies or possible malignancies, since most research indicates lasers have a biostimulatory effect.
CLINICAL APPLICATIONS
Low-intensity laser therapy can be used for differential movement of teeth.
In cases of midline shift, it can be used to stimulate OTM on the opposite side.
Application of low-intensity laser therapy only on teeth to be moved conserves the anchorage. Because low-intensity laser therapy stimulates tooth movement by altering the biologic response and not by increasing forces or changing mechanics, it does not tax the anchorage.
A few studies have reported a decreased rate of tooth movement in adult patients due to decreased vascularity and cellularity of bone.
With increasing number of adult patients in orthodontic practices, low-intensity laser therapy will be beneficial in adult because it increases the vascularity and cellularity of bone.
FUTURE SCOPE AND RESEARCH
Further studies are required to study the efficacy of LILT during comprehensive orthodontic treatment for reducing the treatment time. and effect of LILT on periodontal tissue remodeling during relapse and retention of orthodontically moved teeth.
Source of Support:
Nil.
Conflict of Interest:
None declared.
References
- Electric currents, bone remodeling, and orthodontic tooth movement. Am J Orthod. 1980;77:14-32.
- [Google Scholar]
- Clinical application of prostaglandin E1 (PGE1) upon orthodontic tooth movement. Am J Orthod. 1984;85:508-18.
- [Google Scholar]
- The effect of prostaglandin E2 and calcium gluconate on orthodontic tooth movement and root resorption in rats. Eur J Orthod. 2003;25:199-204.
- [Google Scholar]
- Periodontal tissue activation by vibration: Intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats. Am J Orthod Dentofacial Orthop. 2008;133:572-83.
- [Google Scholar]
- Aspirin, acetaminophen, and ibuprofen: Their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006;130:364-70.
- [Google Scholar]
- Fundamentals of dental lasers: Science and instruments. Dent Clin North Am. 2004;48:751-70. v
- [Google Scholar]
- Stimulatory effects of low-power laser irradiation on bone regeneration in midpalatal suture during expansion in the rat. Am J Orthod Dentofacial Orthop. 1997;111:525-32.
- [Google Scholar]
- Low-level laser irradiation facilitates fibronectin and collagen type I turnover during tooth movement in rats. Lasers Med Sci. 2010;25:25-31.
- [Google Scholar]
- Low-energy irradiation stimulates formation of osteoclast-like cells via RANK expression in vitro. Lasers Med Sci. 2006;21:24-33.
- [Google Scholar]
- Poor penetration of infra-red and helium neon low power laser light into the dermal tissue. Acupunct Electrother Res. 1993;18:17-21.
- [Google Scholar]
- Biostimulatory windows in low-intensity laser activation: Lasers, scanners, and NASA’s light-emitting diode array system. J Clin Laser Med Surg. 2001;19:29-33.
- [Google Scholar]
- Comparison of single and multiple applications of GaAlAs laser on rat medial collateral ligament repair. Lasers Surg Med. 2004;34:285-9.
- [Google Scholar]
- Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: A preliminary study. Lasers Surg Med. 2004;35:117-20.
- [Google Scholar]
- Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: A clinical investigation. Am J Orthod Dentofacial Orthop. 2012;141:289-97.
- [Google Scholar]